REVENUE CYCLE MANAGEMENT
StrateqEHR’s embedded Revenue Cycle Management is designed to maximize your claim reimbursement across all of your care settings. StrateqEHR is tightly integrated with Waystar to provide near seamless integration leveraging the best of both systems. We provide all the tools your team needs to ensure your organizational financial health. We also provide services to augment your revenue cycle staff or to assist with best practices.
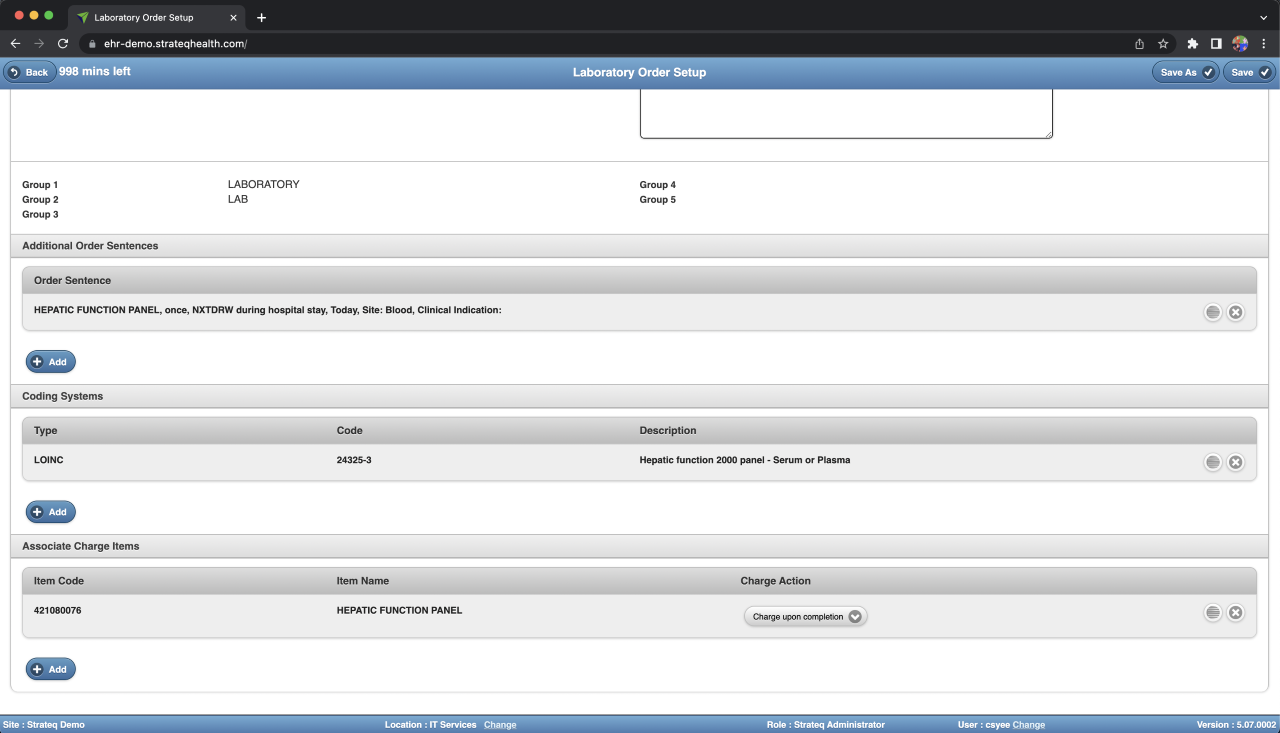
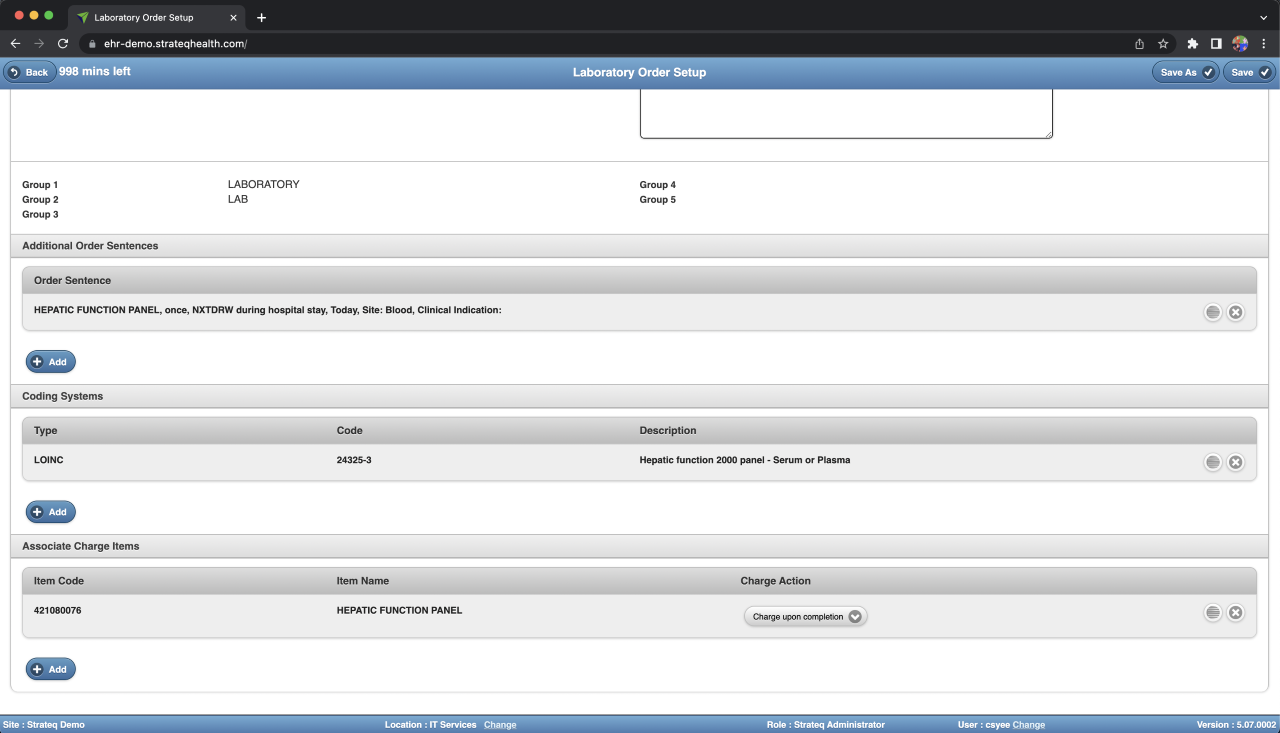
capture critical clinical data
StrateqEHR is uniquely designed to capture critical clinical data elements as well as charges at the point of care, leading to cleaner claims, less denials and faster remits. From eligibility checking to coding to processing claims and managing denials to real-time GL journal entries, and everything in between, Strateq Health has your revenue cycle covered.
features
Eligibility Checking
Real-time eligibility is available from within StrateqEHR leveraging Waystar’s connection to hundreds of Payers. Eligibility results are returned from Waystar and stored in StrateqEHR.
Embedded Coding
StrateqEHR is integrated with 3M CRS to provide an effortless coding process. Once coding is complete, a claim is automatically created after a defined bill hold period.
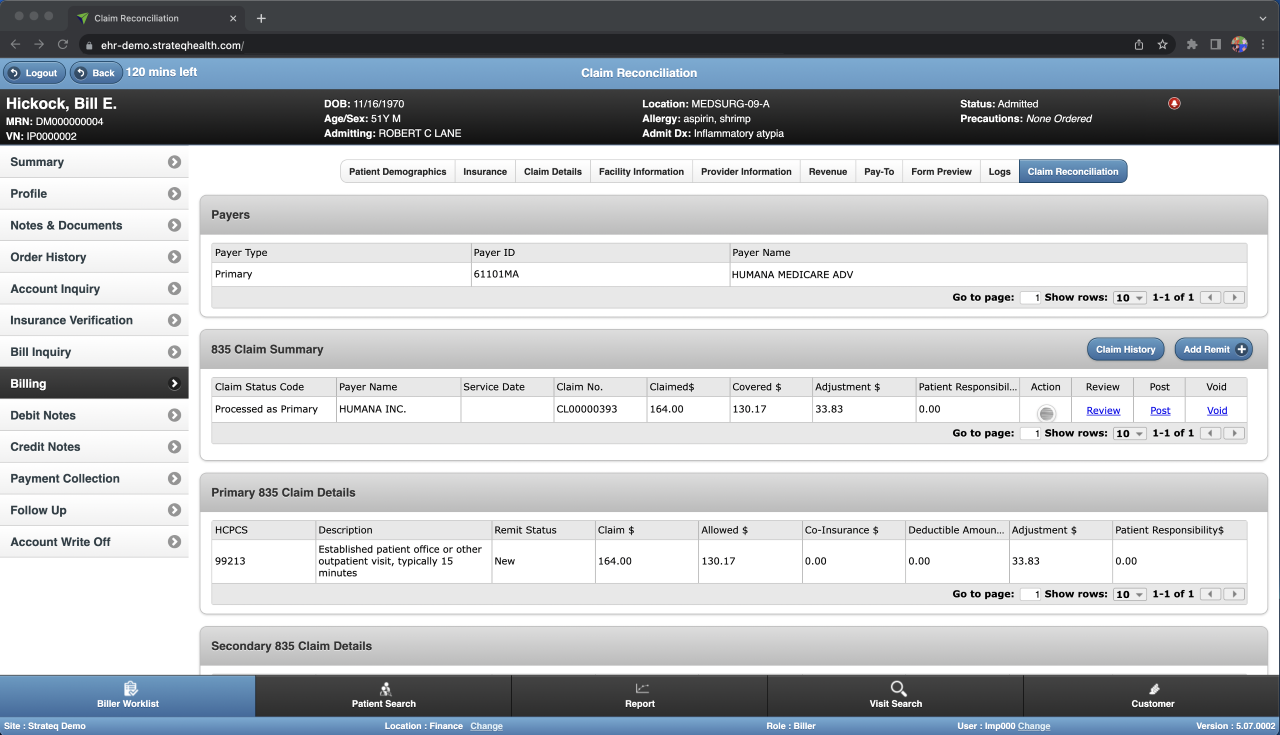
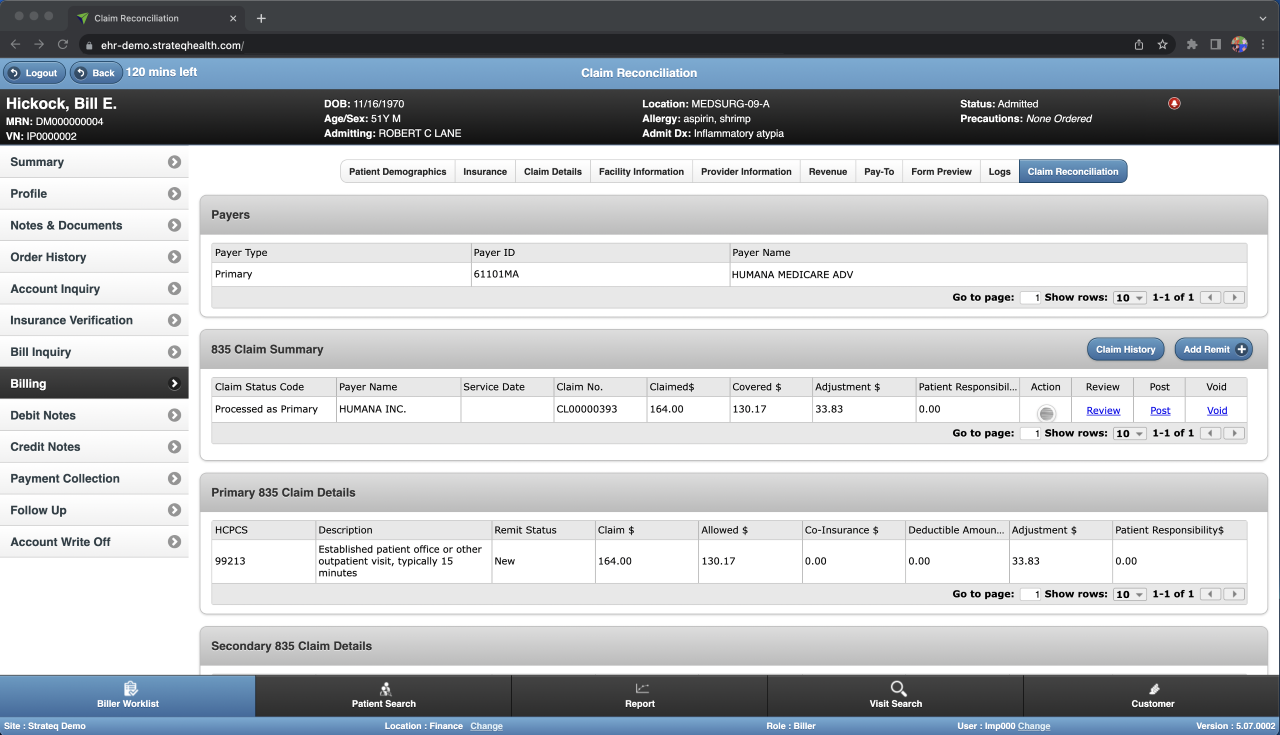
Remittance Processing
Remits received from Payers are automatically sent from Waystar to StrateqEHR for posting to the Patient account. StrateqEHR also supports entering paper remits if an electronic remit isn’t available from a Payer.
Denial Management
The Waystar Denial Management tool is used to process claim denials. Pre-defined Denial templates are available to speed the denial process. You have the option of including clinical information from StrateqEHR if required by a Payer for a denial.
Statement Processing
StrateqEHR sends patient statement data to Waystar on a scheduled basis to send customized statements to your Patients via email or USPS.
Credit Card Processing
Patient payments may be recorded directly in StrateqEHR. Credit Card and Checks are authorized in real time and are posted to the Patient’s account.
Claim Management
Claims are automatically submitted electronically to Waystar on a daily basis. You may use the powerful Claim Management module in Waystar to process and submit claims to payers.
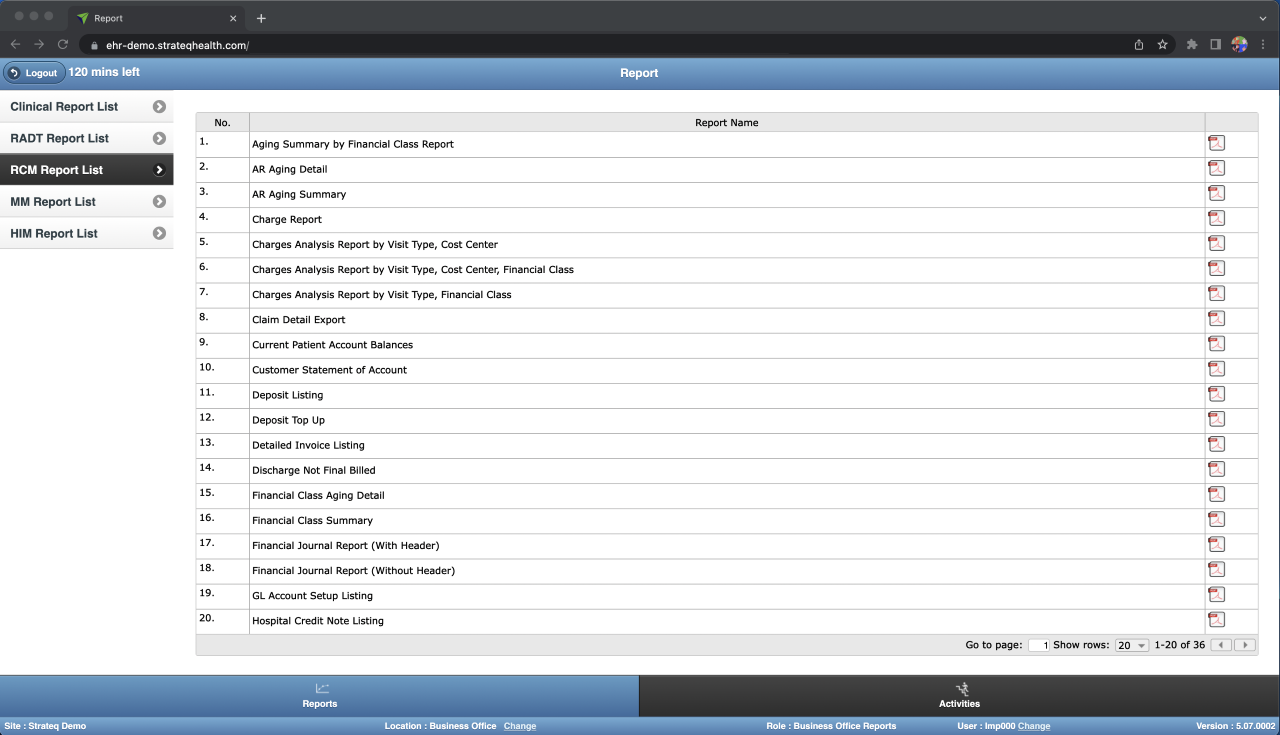
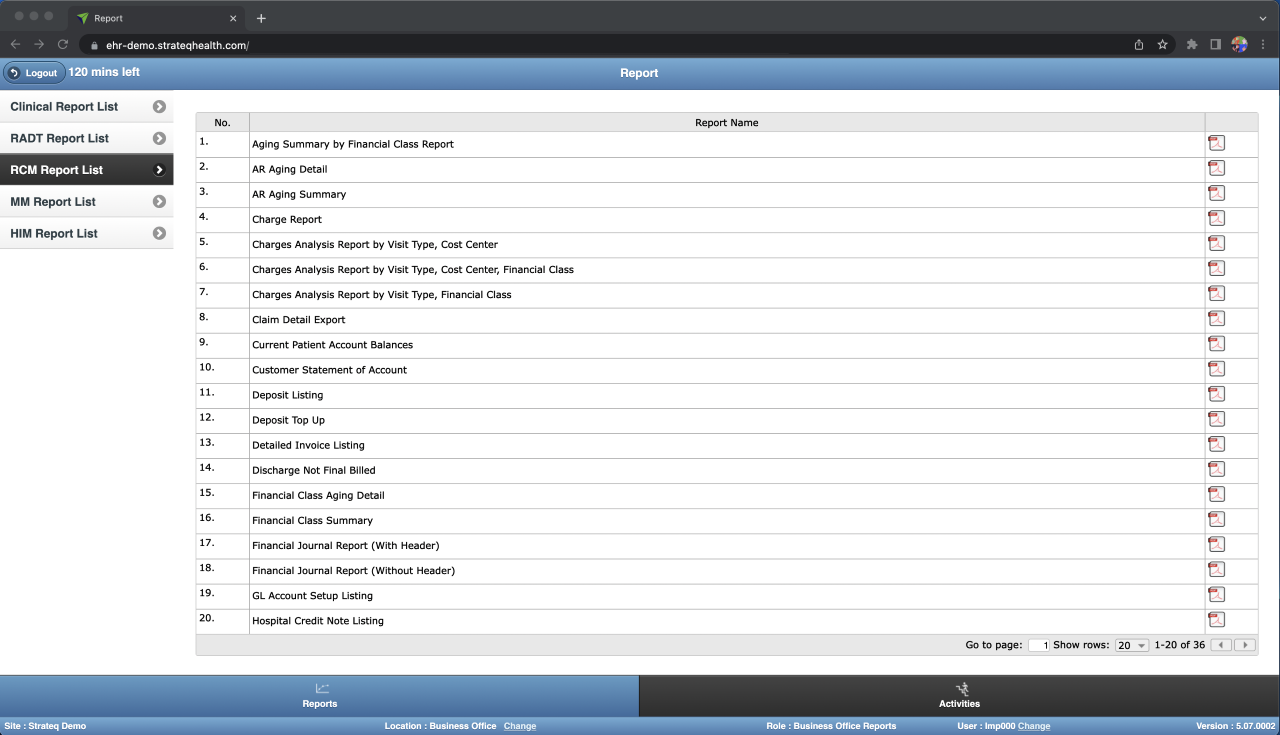
Comprehensive Reporting
Combining reporting capabilities between StrateqEHR and Waystar provides a large set of pre-defined reports for patients accounts, claims, remittance, and payer reporting.
Patient Financial Experience
Using the Waystar Patient Portal, Patients may submit payments via Credit/Debit Card which are then automatically sent to StrateqEHR to post to the Patient account.
Revenue Intergrity
All remits, payments, and credits are exchanged between StrateqEHR and Waystar daily to keep the Patient account balance in sync. This allows payments to be made in either StrateqEHR or Waystar.

